Colorectal Cancer:
The large intestine or large bowel is a part of digestive passage of human body. The rectum is the passageway that connects the large bowel to the anus. When cancer starts in the colon or rectum, it is called colorectal cancer
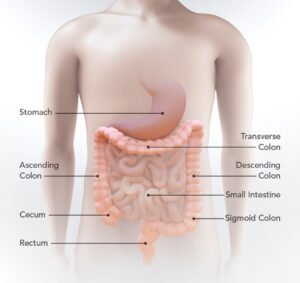

Colon cancer generally affects elderly age group, though it can happen at any age. It usually begins as a small, noncancerous (benign) clumps of cells called polyps that form on the inner layer (mucosal layer) of the colon. As the time passes, some of these polyps can become cancers
Risk factors:
Factors that may increase your risk of colon cancer include:
- Older age. Colon cancer can be diagnosed at any age, but a majority of people with colon cancers are older than 50 years of age. One notable change is the rates of colon cancer in younger population is increasing.
- African-American race. African-Americans have a greater risk of colon cancer than do people of other races.
- A personal history of colorectal cancer or polyps. If one already had colon cancer or noncancerous colon polyps, then he or she is at greater risk of developing colon or rectal cancers in the future.
- Inflammatory Bowel Disease. Chronic inflammatory diseases of the colon, such as ulcerative colitis and Crohn’s disease, can increase the risk of having colon cancer.
- Inherited syndromes that increase colon cancer risk. Some gene mutations passed through generations of a family can increase the risk of colon cancer significantly. Only a small percentage of colon cancers are linked to inherited genes. The common inherited syndromes that increase colon cancer risk are familial adenomatous polyposis (FAP) and Lynch syndrome, which is also known as hereditary nonpolyposis colorectal cancer (HNPCC).
- Family history of colon cancer. One is more likely to develop colon cancer if a blood relative has had the disease. If more than one family member is having colon cancer or rectal cancer, the risk is even greater.
- Low-fiber, high-fat diet. Colorectal cancer may be associated with a typical Westernized diet, which is low in fiber and high in fat and calories. Research in this area has had mixed results. Some studies have found an increased risk of colon cancer in people who eat diets high in red meat and processed meat.
- A sedentary lifestyle. People who are inactive are more likely to develop colon cancer. Getting regular physical activity may reduce the risk of colon cancer.
- Diabetes. Many studies have found that, people with diabetes or insulin resistance have an increased risk of colon cancer.
- Obesity. People who are obese have an increased risk of colon cancer and an increased risk of dying of colon cancer when compared with people considered normal weight.
- Smoking. People who smoke may have an increased risk of colon cancer.
- Alcohol. Heavy use of alcohol increases your risk of colon cancer.
- Radiation therapy for cancer. Radiation therapy directed at the abdomen to treat previous cancers increases the risk of colon cancer.
Signs and symptoms of colon cancer include:
- A persistent change in bowel habits, including diarrhea or constipation or a change in the consistency of stool.
- Rectal bleeding or blood in stool.
- Persistent abdominal discomfort, such as cramps, gaseous distension or pain.
- A feeling that your bowel doesn’t empty completely.
- Weakness or fatigue.
Diagnosing colon cancer:
- Digital Rectal Examination: By doing digital examination, cancer surgeon can find growth in the lower rectum and anal canal. Punch biopsy can be taken easily from the growth to establish the diagnosis
- Proctoscopy: By inserting special instrument rectal growth can be seen and biopsy can be obtained
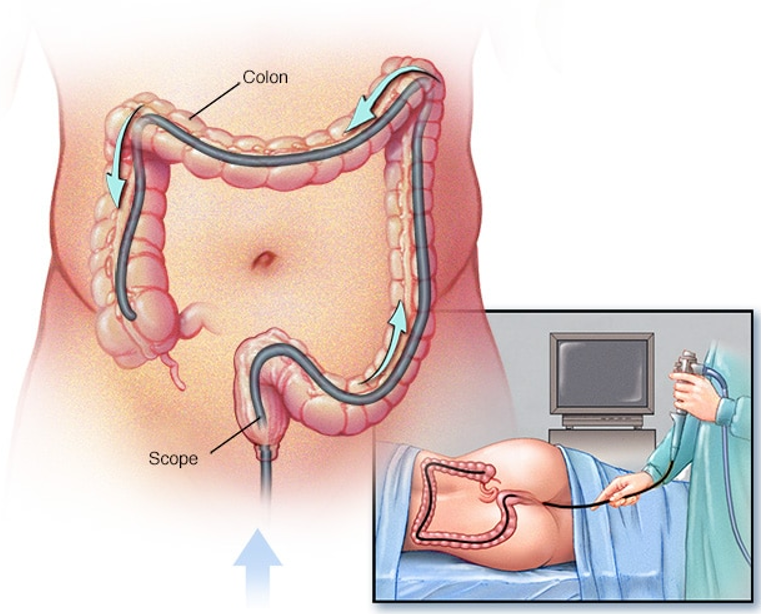
- Colonoscopy : Colonoscopy uses a long, flexible and slender tube attached to a video camera and monitor to view the entire colon and rectum. If any suspicious areas are found, your doctor can pass surgical tools through the tube to take tissue samples (biopsies) for analysis and remove polyps.
- Biopsy. Tissue diagnosis is the only way to make a definitive diagnosis for colorectal carcinoma. Tissue biopsy is a must before starting any treatment in colorectal cancer.
- Blood tests. No blood test can establish colon cancer definitively. But your doctor may test your blood for clues about your overall health, such as kidney and liver function tests
- CEA: Your doctor may also test your blood for a chemical sometimes produced by colon cancers (carcinoembryonic antigen or CEA). Tracked over time, the level of CEA in your blood may help your doctor understand the prognosis and whether the cancer is responding to treatment
- Radiology: If you’ve been diagnosed with colon cancer, doctor may recommend tests to determine the extent (stage) of the disease. Staging helps determine what treatments are most appropriate for you. CT, MRI are routinely done to see the local and regional extent of the disease and PET CT done to see the distant metastatic disease.
Staging:
The stages of colon cancer are indicated by Roman numerals that range from 0 to IV, with the lowest stages indicating cancer that is limited to the lining of the inside of the colon. By stage IV, the cancer is considered advanced and has spread (metastasized) to other areas of the body. The disease which is localized to the colon or rectum is fairly curable.
Screening:
Colorectal cancer is one of the leading cause of cancer related death worldwide. Colorectal cancer screening saves lives. Screening can find precancerous polyps, abnormal growths in the colon or rectum that can be removed before they turn into cancer. Screening also helps find colorectal cancer at an early stage, when treatment works best. Doctors generally recommend that people with an average risk of colon cancer begin screening around age 45. But people with an increased risk, such as those with a family history of colon cancer should consider screening sooner.
For screening, a full-length colonoscopy is often advised to see the entire colonic mucosa, wheather there is any abnormality in mucosa, color change, any polyp or frank growth. If any abnormality found, biopsy can be done in the same sitting.
Treatment:
Treatment depends upon the stage of the disease, location of the tumor and general condition of the patient. The mainstay of treatment is to remove the cancerous mass. Other treatments include chemotherapy, radiotherapy, targeted therapy and immunotherapy.
Surgery:
Surgery generally recommended in early-stage disease and is the only option of cure. It is also done in cases with locoregional disease after neoadjuvant chemotherapy and radiotherapy. Here a part of colon or rectum, or entire rectum is removed depending on the location of the tumor. Along with the colon, its mesentery and draining lymph node stations are also removed
Surgery can be done with open technique, laparoscopic technique or robotically. Robotic surgery in colorectal cancers is in many ways better than laparoscopic surgery and equally effective as open procedures. It leads to early recovery after surgery
Surgery for Early stage disease:
- Polypectomy: If the cancer in the colon or rectum is a small polypoidal mass and localized to it, then removal of the polyp entirely can be done while performing colonoscopy and it can be curative
- Endoscopic Mucosal Resection: Larger polyp may be removed along with the inner layer of colon and rectum using special instruments and technique called endoscopic mucosal resection.
- Minimally invasive Surgery: Polyps that can’t be removed during colonoscopy can be removed using Laparoscopy or Robotic technology. Robotic Surgery now a days becoming standard of care for many of the colorectal cancer cases. In minimally invasive procedures, surgeons perform operation through multiple small holes made in the abdomen, inserting instruments in your abdomen, visualizing colorectal area and growth with the help of a camera and performing surgery. Robotic technology can provide high precision 3 D visualization of the surgical field, hence the blood loss is minimal with preservation of the critical structures.
Various forms of colectomies can be done depending upon the location of the tumor eg. Right and Left Hemicolectomy, Total Colectomy. Similarly for the Rectal cancers, Anterior resection, Low anterior resection, Ultra-low anterior resection or Abdominopelvic resections can be performed. Robotic technology has got advantage over other procedures in deep pelvis in cases of rectal cancers. - Open technique: All these procedures can be performed through open technique also after making an incision in the abdominal wall.
- Lymphadenectomy: Nearby draining lymph nodes are also removed during the procedures which may harbor cancerous cells.
Surgery for more advanced disease:
Many patients present with advanced stage who requires chemotherapy and/or radiotherapy (called Neoadjuvant) before proceeding to Surgery. This is to downgrade the tumor. All the above mentioned procedures can be performed after neoadjuvant therapy
If the stage of the cancer is very advanced, patient’s general condition is not good and patients present with bowel obstruction, in that case your surgeon may recommend an operation to relieve the blockage called ileostomy or Colostomy. This may help in relieving the symptoms. In these situations, surgery is not done to cure the disease but to relieve the patients from obstruction, bleeding or pain.
Surgery in metastatic Setting:
When the cancer has spread to other organs of the body, it is called metastatic disease. In metastatic colorectal cancers, if the patient’s general condition is good and there is limited numbers of metastatic lesions in Liver or Lungs, your surgeon may offer surgery for the disease with curative intent. In these situations, chemotherapy is generally required before or after the surgery.
Chemotherapy:
These are drugs to kill cancer cells. Chemotherapy for colon cancer is usually given after surgery if the cancer is larger or has spread to the lymph nodes. In this way, chemotherapy will kill any cancer cells that may remain in the body and help reduce the risk of cancer recurrence
Chemotherapy used before an operation is called neoadjuvant chemotherapy. The intention is to shrink a large tumor so that it can be removed entirely with surgery.
Chemotherapy can also be used to relieve symptoms of colon cancer that can’t be removed with surgery or that has spread to other areas of the body. Sometimes it’s combined with radiation therapy.
For some people with low-risk stage III colon cancer, a shorter course of chemotherapy after surgery . This approach may reduce the side effects compared with the traditional course of chemotherapy, and may be just as effective.
Targeted drug therapy:
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die. Targeted drugs are usually combined with chemotherapy. Targeted drugs are typically reserved for people with advanced colon cancer
Immunotherapy:
It is a drug treatment that uses your immune system to fight cancer. Your body’s disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that blind the immune system cells from recognizing the cancer cells. Immunotherapy works by interfering with that process. Immunotherapy is usually reserved for advanced colon cancer. Your doctor might have your cancer cells tested to see if they’re likely to respond to this treatment.
Radiotherapy
Radiation therapy uses powerful energy sources, such as X-rays and photons, to kill cancer cells. It might be used to shrink a large cancer before an operation so that it can be removed more easily. Sometimes it is used after surgical resection of the tumor. When surgery isn’t an option, radiation therapy might be used to relieve symptoms, such as pain
